What is antibody humanisation and what are the main differences between chimeric, humanised and fully human antibodies? An overview of what we learned from our discussions with Olivier Léger, an expert in antibody engineering with over 25 years’ experience in the field.
What is antibody humanisation and what are the main differences between chimeric, humanised and fully human antibodies?
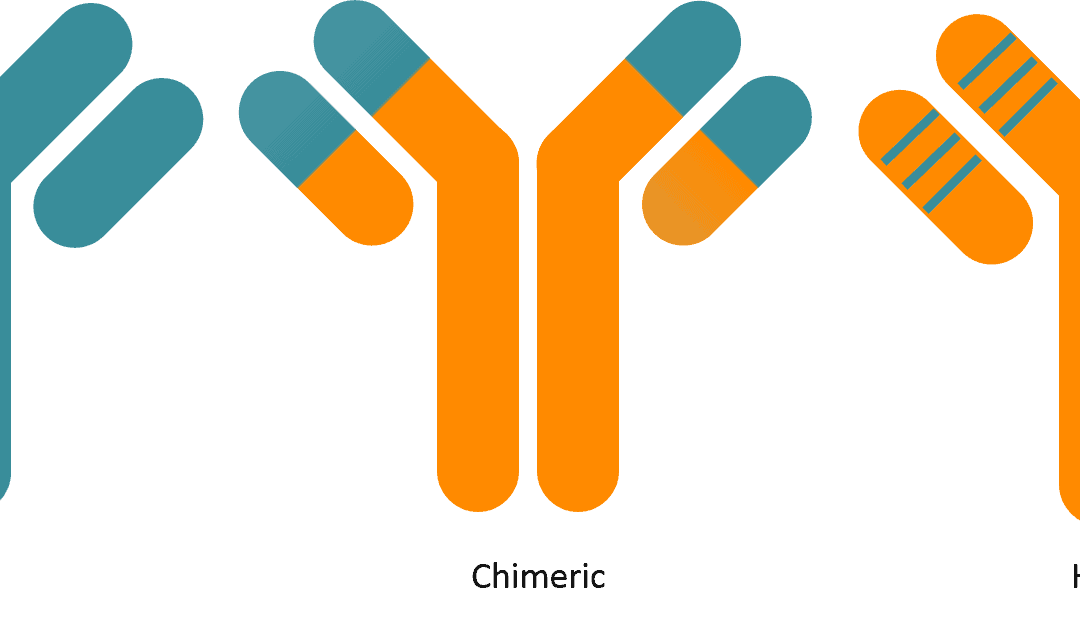
In 2014, the WHO (World Health Organisation) issued new guidelines redefining the different categories of therapeutic antibodies. Its INN (International Nonproprietary Names) antibody drug nomenclature divides therapeutic antibodies into 3 categories:
- chimeric or “-ximab”
- humanised or “-zumab”
- fully human or “-umab”
Classifying a given antibody based on WHO nomenclature requires a sequence alignment between the antibody and the human germline sequences in the IMGT reference database. If the sequence identity is under 85%, the antibody is a -ximab, and above 85% it’s either a -zumab or -umab. -zumabs and -umabs can’t be differentiated based on percent identity. The difference comes from the origin of the antibody. An antibody derived from a murine (or more generally non-human) sequence will be classified as -zumab and one with a human origin (phage display, transgenic mice or B-cell cloning techniques) as -umab.
In a standard project, a mouse antibody BLASTed against the IMGT databank would usually show around 65-80% identity to the closest human germline in the VL domain and 60-75% in the VH domain. Reaching the required identity rate in the VH domain will therefore often require mutating some residues in the CDRs.
In the original definition, brought about by Kabat, zones defined as CDR are more extensive than in that of the IMGT. IMGT defined CDRs on the basis of structure alignment of immunoglobulins and T-cell receptors. This difference in annotation is important, as a residue can be considered as being part of the CDR with the Kabat annotation, when with the IMGT annotation it is not.
Mutations in the CDRs (as defined by Kabat) are therefore required in the humanisation process in order to reach 85% identity in VH domains. These mutations used to be avoided, but they’re no longer a no-go. The change in nomenclature means that most so-called -zumab (and therefore humanised) antibodies on the market would no longer be allowed this label. They would now be considered -ximab. In the same way, some “fully human” antibodies (in particular those derived from phage display libraries, that have sequences with numerous mutations compared to the germline sequences) would now no longer be allowed the “fully human” designation given their below 85% identity.
With this change in nomenclature, an 85% identity objective with the closest germline must be targeted in a project aiming for the -zumab designation. This distinction between chimeric and humanised might prove extremely important to convince investors; therefore the WHO guidelines must systematically be aimed for.
What is CDR grafting? Why is humanisation more complex than sequence alignment?
First of all, I must remind you of what CDRs are. Let’s put ourselves in the context of the Kabat definition. CDRs are the hypervariable regions responsible for antigen binding. There are 3 CDRs (CDR1, CDR2, CDR3) per chain of an antibody.
The variable domain of a light chain is encoded by two rearranged genes (V for variable and J for junction). Humanisation mainly involves the sequence identity of the V gene. The part of the J gene that doesn’t code for CDR3 is very identical between species and humanising it does not present any difficulties. CDR3 is formed by the V-J junction. Therefore here, the V gene codes for CDR1, CDR2 and two thirds of CDR3.
The variable domain of a heavy chain is encoded by 3 genes: V (variable), D (diversity) and J (junction). CDR3 is created by the V-D-J junction. That’s why CDR3 of the heavy chain shows a high variability in length as well as in amino acid composition. Finally, it is the combination of all 6 CDRs that really constitutes the paratope and defines the specificity of the antibody. The binding interfaces between antigen receptor molecules and their ligands are generally large (over 1,500 Å2) and 10–30 side chains from each side make close contact. However, despite the broad interface seen in the crystal structures, sequence diversity in antigen receptors is not evenly distributed among all 6 CDRs but is highly concentrated in the CDR3 region of the VH. Therefore, carrying out mutations in the CDR loops can generate a loss of affinity of the antibody for its antigen.
So CDR grafting is the transplantation of CDRs from the original (mouse monoclonal) antibody into a human framework. Immunoglobulin domains have a beta-sheet structure. In the VH and VL domains, CDRs form loops that link the beta sheets together. It is these loops that bind with the antigen. They are hypervariable, which one might think indicates that they adopt very variable tridimensional structures. However, in the end, analysis of available antibody structures shows that their structural diversity is fairly restricted.
These defined structures are imposed by a number of residues outside the CDRs (in the framework regions), which come into contact with some residues from the loops, playing a key structural role. That’s where the difficulty lies in the process of CDR grafting. Taking murine CDRs and transplanting them directly onto the most homologous human backbone won’t work. Residues from the framework regions, which ensure the formation of loops, must be maintained, or loop formation will be altered and the shape of the paratope modified.
Murine residues to be kept are those that maintain loop conformation, but also those that play a role in the interface between the variable regions of the heavy chain and the light chain. VL and VH are two domains that interact without forming a covalent bond. The interaction between the two domains is maintained through hydrogen and electrostatic bonding. The residues involved in this interaction must also be maintained, or the paratope might be modified and the antibody affinity altered.
The loops to be transplanted must be defined and placed in a human germline framework. Then, a structural model is created in order to evaluate which of the murine sequence residues must be kept for good loop conformation to be maintained. When determining sequence homology to human germlines through a BLAST search, the heavy chain CDR3 doesn’t not come into account at all. There is therefore no attempt to humanise it. However, there are certain conformations of CDR1 and CDR2 specific to the mouse that don’t exist in humans; but most of the time, canonical conformations of the CDRs are common between the two species.
Why are “back mutations” necessary?
Back mutations are precisely the critical residues from the framework regions of the mouse antibody that must be kept in order to maintain the right conformation of loops. A humanisation project should at first aim to be very conservative. Some framework residues are seen as critical and they will be kept murine. Others – called Vernier residues – are of more questionable importance. This is where molecular modelling helps.
A model of the Fv regions (Variable Fragment = VH+VL) is created for each antibody through sequence homology to crystal structures published in the PBD (Protein Data Bank; with over 2,500 structures available in the PDB, a high-fidelity molecular model is generally obtained) with a view to assessing whether those residues can be changed. In the case of a 90% confidence level that modifying them won’t have an impact on conformation, it can be attempted. In the absence of molecular modelling, an even more conservative attitude would be adopted and the initial humanisation variants would not include any modification of the Vernier residues, which would lengthen the duration of the process to reach the 85% objective. Here, molecular modelling allows for a faster humanisation process.
So the benefit of molecular modelling lies in minimising the number of variants for a given human germline that is used for humanisation?
That’s not its only value. Observing the lateral chains of CDR residues gives us an understanding of the shape of the paratope (the surface that interacts with the antigen). The core binding region is CDR3, while CDR1 and 2 are more peripheral. Depending on the antibody being humanised, it is not necessary for all 6 CDRs to bind with the antigen.
Molecular modelling gives an indication of whether or not a given lateral chain has a high probability of being involved in the interaction with the antigen. If the lateral chain of interest is directed towards the core of the antibody, it will be kept if it plays a structural role. If it’s directed towards the paratope, it could bind with the antigen, or if it’s directed towards the solvent (away from the paratope), it could be concluded that it’s possible to mutate the corresponding residue. There are therefore two main draws to molecular modelling: it makes it possible to identify the framework residues to keep, but also, in the CDRs, the residues that can be substituted for the corresponding human germline residue.
Does humanisation optimise antibody properties? (affinity, aggregation)
Humanisation projects used to involve BLASTing against the IMGT bank and to use the most homologous human germline to create the humanised version from this germline only. Now we know that each germline family presents different physicochemical properties. According to works by Andréas Plückthun’s group in the 90s, it’s broadly possible to say that odd-numbered subgroups (1, 3, 5 and 7) have better physicochemical properties than even-numbered subgroups (2, 4 and 6).
However, let’s not forget that CDRs represent an important part of the sequence. They will therefore have an influence on the physicochemical properties of the molecule. So this is merely a trend, the idea being to use the germline that presents the strongest homology, but to also test others, even if they show lower homology.
For example, the IGHV3-11 subgroup will be used preferentially because it is known for having good physicochemical properties and it constitutes a large part of the antibodies present in humans. Generally, in a humanisation project, 3 separate germlines will be selected for the heavy chain (HC) and 3 for the light chain (LC). The 9 possible HC / LC combinations of these germlines will then be created, followed by an analysis of the level of expression of the supernatant (transient expression in HEK293 or CHO), the aggregation rate by SE-HPLC, the SDS-PAGE profile under reducing or nonreducing conditions, and their thermostability profiles (Differential Scanning Calorimetry, DSC) in order to determine the fusion temperatures of the CH2, CH3 and Fab domains of each humanised version.
It is this last analysis that is of interest in order to compare the stability of the chimeric versions to the various humanised versions. For example, in our last two projects, we were able to increase the Tm of the Fab from 70°C for the chimeric antibody to 80°C for the humanised antibody. Of course, the impact of mutations on the Tm cannot be predicted, hence why several combinations are tested.
After this step in the process, it’s possible to say that a humanised antibody has been generated that presents optimised physicochemical characteristics. For me, this is the main reason for antibody humanisation. Immunogenicity is indeed a multifactorial issue. We now know enough to understand that there isn’t a real difference in immunogenicity between humanised antibodies and those called “fully human”.
Other factors come into play, in particular the physicochemical properties of the molecule. The amount of aggregates must be minimised. Guidelines now dictate that the percent of aggregate must be below 5%, however we also know that aggregates are the number one enemy when it comes to immunogenicity. The humanisation rate is therefore no longer the main criterion by which the successful humanisation of an antibody is judged. The physicochemical properties are.
You mentioned examples where the different variants that were tested had a significant influence on physicochemical properties. Can a similar impact be observed on their differences in terms of affinity?
The first phase of a humanisation project must consider the expression, stability, aggregation but also affinity and biological activity criteria. It’s of course necessary to check that the biological affinity and activity are at least equivalent to those in the chimeric form. This first phase is a time to be conservative. Critical murine residues to be kept will be identified (the so-called back mutations) in order to maximise the chances of a good affinity for the antigen.
The second phase sees an exploration of the possibility of mutating those residues in order to obtain a better sequence homology, over 85% if possible for the VH and the VL. It’s generally easier to obtain 85% homology between the humanised version and the closest human germline sequence for the VH than for the VL. For the VH, close to 80% is generally obtained. Knowing that there are about 98 residues for the VH, reaching 85% means substituting another 4 or 5 murine residues for their counterparts from the corresponding human germline chain. This is only possible through substituting the residues in CDR1 and CDR2.
Might humanisation have an impact on ADAs (Anti Drug Antibodies)?
ADAs are mainly directed against CDRs. So, whether in the presence of a fully human, humanised or chimeric antibody, there is always a response against CDRs. As they are unique (in particular the heavy chain CDR3), injecting an antibody for a long amount of time will necessarily end up inducing an anti-CDR response. This has been very well documented, notably in the anti-TNF field. This is why there’s a large number of them on the market.
Some patients can have a hyper-boosted immune system which will induce a premature response to the antibody. In this case, a second antibody will be administered, and so on, if it happens again. This response is inevitable. There are in silico approaches that aim at minimising it, such as research into T cell epitopes. In a CDR grafting humanisation project, it’s possible to include such a step. Some companies offer this service, including Lonza, EpiVAX and Abzena. It’s also possible to conduct a functional in vitro study using dendritic cells to identify the generated peptides. This approach is, however, very heavy and costly.
In summary, is the true interest of humanisation vis-à-vis ADAs mainly the gain in terms of physicochemical properties, notably when it comes to aggregation?
Absolutely. A recent article has illustrated this point by showing that ADAs are generally directed against the CDRs and so from this point of view, there isn’t a difference between a humanised antibody and a fully human one.
Are there any differences between humanisation approaches?
As we’ve seen, the de-immunisation approach is yet to prove itself. There are also phage display techniques, the archetypical example being HUMIRA® which remains the therapeutic antibody which generates the highest turnover among all those on the market. It’s originally a mouse antibody which was humanised through phage display. It was developed by CAT (Cambridge Antibody Technology). To my knowledge, they are the only ones to have managed the feat of changing the sequence as a whole (including CDR3 of the heavy chain) while keeping the specificity of the mouse antibody.
More frequently, the teams that carry out this approach start from human libraries of heavy and light chains and preserve the murine CDR3 of the heavy and light chains. These libraries are selected through phage display against the epitope. Fully human antibodies are obtained this way. These techniques are very time consuming and heavy.
Unlike the modernised CDR-grafting technique we’ve discussed, these techniques are not based on optimising physicochemical properties. What’s more, some binding points may be lost and others created during the selection process, creating a risk of changing the epitope (epitope drift). This can have harmful consequences on the biological activity and conservation of cross-reactivity with the antigen of species other than human.
Should all new antibodies in development be humanised? Or are there any cases where the development of a chimeric antibody is still a relevant approach?
It all depends on what is meant by chimeric. Some chimeric antibodies have a high humanisation rate right from the start and can present very good physicochemical properties. In this case, it may not in theory be indispensable to proceed to their humanisation. When it comes to convincing an investor however, it may be difficult to persuade them do without humanising the sequence. They may well say “A ximab? Oh no, not a ximab. Why did you not generate a zumab?” So we must not be deluded, there is a real scientific interest but also a commercial one to the humanisation of an antibody. But in conclusion, I must stress that my experience has shown that in two out of three cases, humanisation really improves the starting molecule.
Many thanks to Olivier Leger for having answered our questions!